What are the effects of prolonged pressure on tissue? – Introducing the damage cascade.
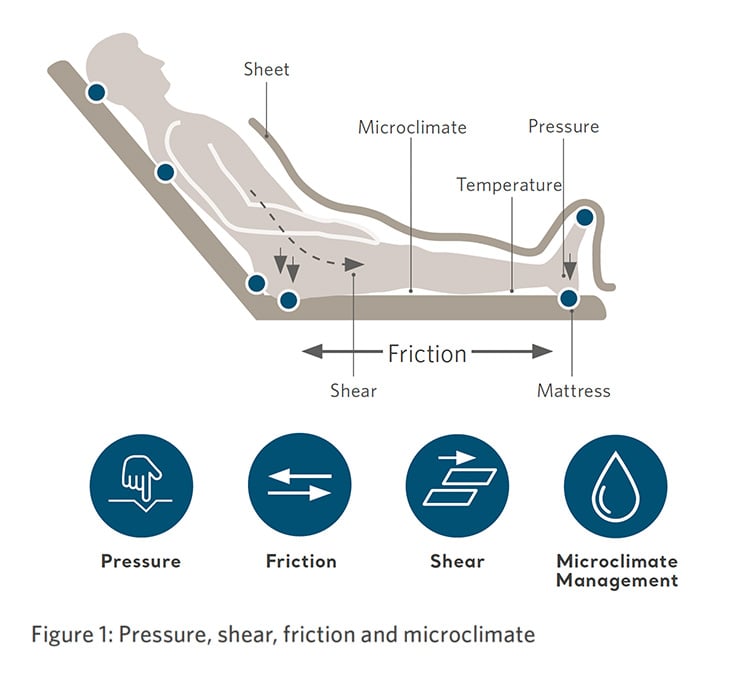
The principle causes of pressure injuries are pressure, friction, shear, moisture, and tissue deformation1–3 (figure 1). Pressure injuries develop over time, they do not appear on the skin instantaneously4 instead there is a sequential and gradual deterioration of cell structures which are subjected to bodyweight or external forces5.

 Pressure induced tissue damage occurs when too much pressure is applied to an area of the body for a prolonged period of time, resulting in small blood vessel collapse and ischaemia, or a restriction of blood supply and lymphatic flow to the tissues. Tissue damage is often more common over bony prominences, since the pressure may be 3–5 times greater than in tissues not affected by bony structures6,7.
Pressure induced tissue damage occurs when too much pressure is applied to an area of the body for a prolonged period of time, resulting in small blood vessel collapse and ischaemia, or a restriction of blood supply and lymphatic flow to the tissues. Tissue damage is often more common over bony prominences, since the pressure may be 3–5 times greater than in tissues not affected by bony structures6,7.
While pressure may be applied to the skin, the effects of pressure are frequently exacerbated by lateral shear forces6,7. Compression of tissue over bony prominences occurs concurrently with shear forces and are a key factor in pressure injury formation8, leading directly to cell death. Skeletal muscle is the most sensitive to pressure9 and prolonged pressure leads to deep pressure-induced tissue damage. The intensity and duration of pressure on deep tissues are key factors in tissue damage10.
Tissue tolerance
The development of a pressure injury also depends on individual tissue tolerance; this is affected by many physical and environmental risk factors. The importance of other factors such as internal anatomy, excess heat and moisture on the skin will have an influence on the individual’s susceptibility to pressure injury formation11.
Evolving insights in pressure injury formation: The damage cascade & the inflammatory response
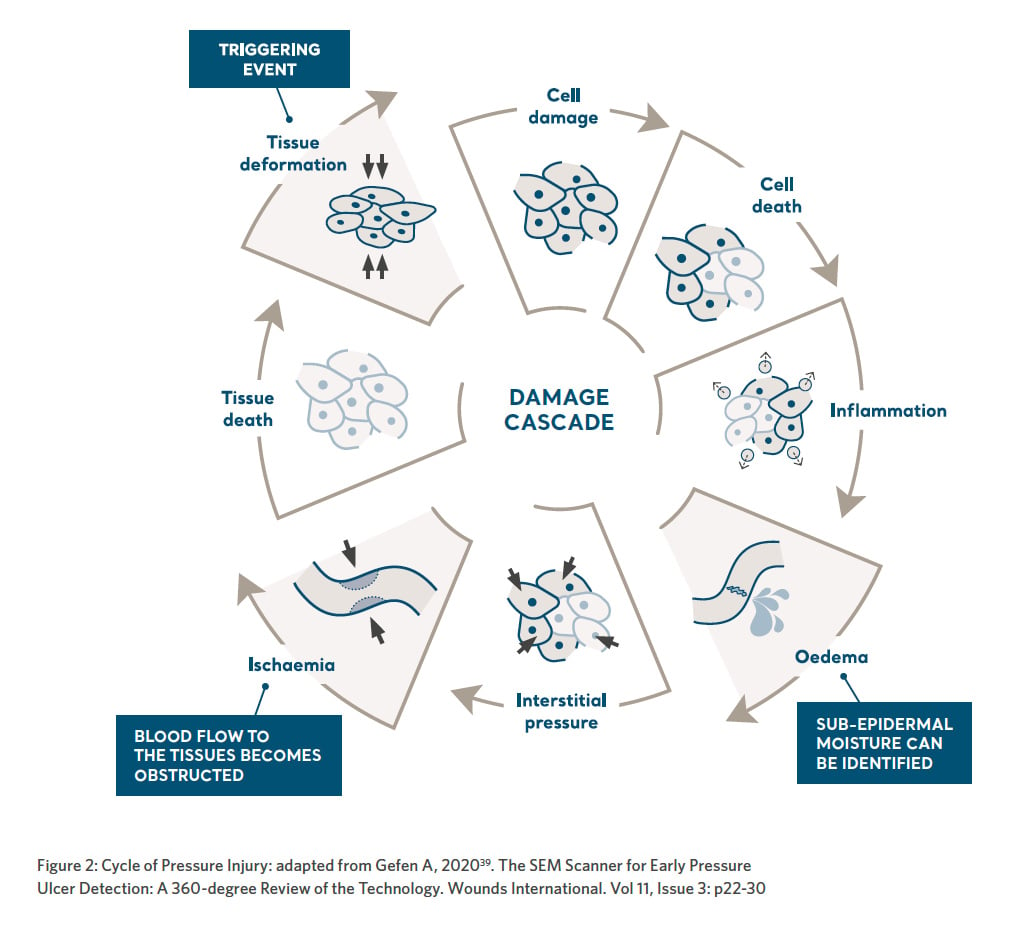
Important insights on how pressure injuries develop and progress in severity have been identified and published in recent scientific work5. This body of knowledge suggest three major contributors to cell damage and tissue necrosis namely: deformation, inflammation and ischaemia in the form of a damage cascade12 (Figure 2).
Direct deformation
Prolonged tissue deformations lead to cell death at a microscopic level beneath the surface of the skin, which subsequently triggers an inflammatory response within the tissues12. Inflammation is the body’s first response to tissue damage and a mechanism to combat injury5. Tissue and cell stresses trigger cellular pathways that initiate inflammation.
A key factor in pressure injury development is the prolonged nature of these stresses which trigger chronic inflammation and over expressed, uncontrolled pathology, including destructive proteinases and an oxidative environment13–15. This lack of control allows inflammation to progress unabated to become harmful rather than helpful to tissue repair.
Learn more about the damage cascade by downloading The Science of Sub Epidermal Moisture below.
The Science of Sub-Epidermal Moisture (SEM) clinical evidence summary
Elevated levels of SEM is a biomarker of early tissue damage that can lead to pressure injury development. SEM can be identified by assessing the biocapacitance of tissue. This noninvasive technology enables early and objective assessment of increased pressure injury (PI) risk, empowering you to take decisive action to minimize PI incidence and to help reduce overall cost and time to care.
Download our Science of SEM clinical evidence summary and learn about:
- The challenges of preventing pressure injuries
- Effects of prolonged pressure on tissue
- The Provizio SEM Scanner hand-held wireless, noninvasive device
- Foundational clinical studies
DOWNLOAD SCIENCE OF SEM CLINICAL EVIDENCE SUMMARY
Talk to an Arjo Expert
Learn more about the Provizio SEM Scanner by speaking with an Arjo Expert, who will respond to your request in a timely manner.
References:
- Brienza D, Antokal S, Herbe L, Logan S, Maguire J, Van Ranst J, Siddiqui A. Friction-induced skin injuries-are they pressure ulcers? An updated NPUAP whaitepaper. J Wound Ostomy Continence Nurs 2015;42:62-4
- Stekelenburg A, Strijkers GJ, Parusel H, Bader DL, Nicolay K, Oomens CW. Role of ischemia and deformation in the onset of compression-indued deep tissue injury: MRI based studies in a rat model. J appl Physiol 2007;102:2002-11
- Celen KK, Stekelenburg A, Loerakker S, Strijkers GJ, Bader DL, Nicolay K, Baaijens FP, Oomens CW. Compression-induced damage and internal tissue strains are related. J Biomech 2008;41:3399-404
- Gefen A (2020). The SEM Scanner for Early Pressure Ulcer Detection: A 360-degree Review of the Technology. Wounds International. Vol 11, Issue 3: P22-30. Figure adapted by permission of Wounds International Ltd
- Gefen A (2018) The future of pressure ulcer prevention is here: Detecting and targeting inflammation early. EWMA Journal 2018, 19(2):7-13
- Orsted HL, Ohura T, Harding K. International review. Pressure ulcer prevention: Pressure, Shear, Friction and microclimate in context. A consensus document. London: Wounds International; 2010
- Ohura T, Takahashi M, Ohura N. Influence of external forces (pressure and shear force) on superficial layer and subcutis of porcine skin and effects of dressing materials: Are dressing materials beneficial for reducing pressure and shear force in tissues. Wound Repair Regen. 2008; 16(1):102-107
- Stekelenburg A, Gawlitta D, Bader DL, Oomens CW. Deep tissue injury: how deep is our understanding? Arch Phys Med Rehabil 2008;89:1410-3
- Oomens CW, Bader DL, Loerakker S, Baaijens. Pressure induced deep tissue injury explained. Ann Bioned Eng 2015;43:297-305
- Agam L, Gefen A. Pressure ulcers and deep tissue injury: a bioengineering perspective. J Wound Care. 2007;16(8):336-42
- European Pressure Ulcer Advisory Panel, National Pressure Ulcer Advisory Panel & Pan Pacific Pressure Injury Alliance. Prevention and Treament of pressure ulcers/injuries:Clinical Practice Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPIA:2019
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: The International Guideline 2019. Emily Haesler (Ed.). EPUAP/NPIAP/PPIA: 2019. Section 2: The Aetiology of Pressure Injuries – Contributors to cell damage and tissue necrosis in pressure injuries, Pages 22-23
- Schultz GS, Davidson JM, Kirsner RS, Bornstein P, Herman IM. Dynamic reciprocity in the wound microenvironment. Wound Reapir Regen. 2011;19:134-148
- Nwomeh BC, Yager DR, Cohen IK. Physiology of the chronic wound. Clin Plast Surg 1998;25:341-356
- Rogers AA, Burnett S, Moore JC, Shakespeare PG, Chen WY. Involvement of proteolytic enzymes-plasminogen activators and matrix metalloproteinases – in the pathophysiology of pressure ulcers. Wound Repair Regen. 1995;3(3):273-83