Pressure injury prevention with Provizio® SEM Scanner: Boston Medical Center case study
Boston Medical Center (BMC) is a private, not-for-profit, 514 bed, level one trauma and academic medical center located in Boston’s historic South End. BMC is the largest safety net and busiest provider of trauma and emergency services in New England with an average of 120,000 ER visits annually. BMC provides the full spectrum of care to pediatric and adult patients that includes a large, under-served population. Over 1,750 nurses provide quality patient care, advocating and educating the diverse patient population.

The challenge
Annually, pressure injuries (PIs) occur in more than 2.5 million US patients,1 of whom roughly 60,000 die due to infection or other sequalae,2 costing US healthcare more than $26.8 billion.3 Patients with dark skin tones are four times more likely to die from PI related causes,4 have a 60% greater risk of PIs than light skin tone patients,5 have a greater risk of multiple PIs6 and suffering worst stage PIs.6 PIs are difficult to prevent because injuries can develop quickly with irreversible damage occurring in vulnerable patients within a matter of hours.7,8 Furthermore, inflammatory changes in the skin and underlying tissues may begin 3 to 10 days before becoming visible.9 The impact of PIs to patients is substantial — reduced quality of life, high levels of pain, loss of independence, reduced mobility, and potential of leading to lifethreatening complications. Facilities incur longer length of patient stay, increased cost of treatment and nursing time, and litigation risk.10
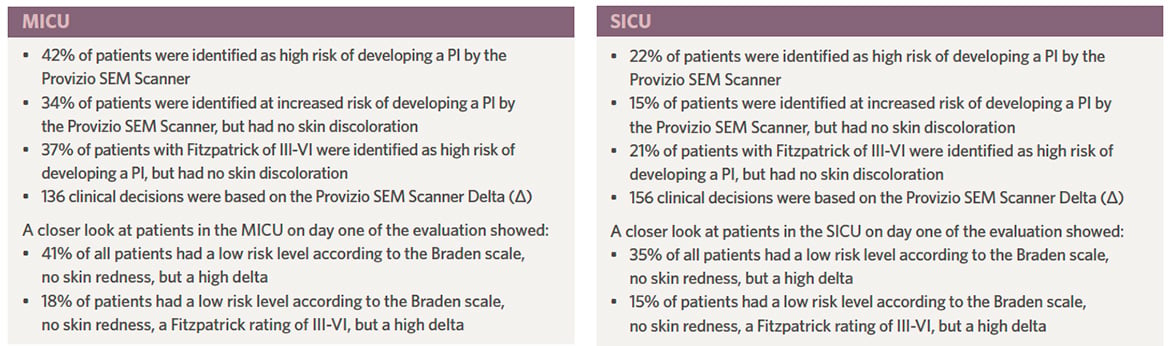
Boston Medical Center faced the same challenges as the rest of the nation which included high staff turn-over, high utilization of travel nurses, inexperienced staff and staffing shortages. The units chosen for this case study include two Medical Intensive Care Units (MICUs) and a Surgical Intensive Care Unit (SICU). Both units have a diverse population with visual skin assessment demonstrating various skin tones and noted inconsistencies in documenting both risk of developing a PI as well as the skin assessment itself. Many of these patients have significant co-morbidities that make them at higher PI risk. BMC identified that the hospital acquired pressure injury (HAPI) rate did not meet the national benchmark and committed to identifying strategies to improve this patient quality measure and decrease unintentional harm to patients.
The approach
The Quality Initiative (QI) Improvement Project commenced in 2021 and was focused on the Critical Care Units. The units selected for the evaluation were chosen due to the high average HAPI occurrences and the desire to reduce pain and injury to patients, and improve quality of patient care. The process included literature reviews, development of a concise AIM statement, process mapping, fishbone development, and inclusion of the Nurse Practice Council and MICU and SICU unit-based councils in the project. Improvements to clinical practice initiated included a pressure redistribution surface trial with subsequent purchase of new critical care beds and surfaces to replace outdated beds. Additionally, education was provided to staff and leaders on the use of sacral foam dressing placement for initial prevention, wedges for offloading, repositioning sheets to assist with patient repositioning, 02 sensors to replace hard ear clips and finger probes as well as external urinary devices for both males and females to reduce moisture associated skin damage. Following the December 2022 prevalence study, the Wound, Ostomy and Continence (WOC) Team at BMC reviewed the literature with the QI Team. That team offered to provide a retrospective data analysis of patients with HAPIs to identify if there was a significant issue with patients and dark tone skin (DTS). This retrospective data analysis identified 64% of the patients had DTS. This led the WOC team to focus on this high-risk group of patients.
Why Provizio SEM Scanner?
In reviewing products available on the market, the decision was made to evaluate the Provizio SEM Scanner, which is referenced in the 2019 International Guidelines for Prevention and Treatment of Pressure Ulcers/ Injuries Clinical Practice Guideline. Sandy Hughes, RN, MSN, CWOCN said the Wound Care team wanted to explore a device that would be an objective measurement of PI risk for all patients. Sandy shared that “pressure injuries are not easily visualized in persons with dark skin tones, especially very dark skin tones. Having a device that can identify increased sub-epidermal moisture changes which is a biomarker for tissue damage will afford all persons, regardless of skin tone, the benefit of earlier pressure injury prevention interventions to prevent further injury.” The Provizio SEM Scanner allows clinicians to identify patients at increased risk of PI 5 days*11 earlier than visual skin assessments, regardless of skin tone.12 Provizio SEM Scanner uses an integrated electrode sensor to compute a delta value from a set of readings made around an anatomical location. A Delta (Δ) of ≥ 0.6 indicates tissue is at increased risk of PI development, a Delta (Δ) of < 0.6 indicates tissue is at lower risk of PI development. This enables objective and anatomically-specific data that works for all skin tones to wound care and bedside nurses performing PI risk assessments. Provizio SEM Scanner also empowers nurses with the ability to deliver timely, anatomically-specific and targeted pressure injury preventive interventions to reduce a patient’s risk of developing a PI.
Provizio SEM Scanner evaluation design
The goal of the evaluation was to reduce PIs, understand ease of use, determine how this device can integrate seamlessly into BMC’s clinical workflow and understand the outcomes of the Provizio SEM Scanner on dark skin tone patients. The evaluation of the device began on May 8, 2023 and concluded on May 17, 2023. Across all ICUs, 111 patients were scanned. Education on the use of the Provizio SEM Scanner included the WOC RN Team to ensure consistent skin assessment, scanning and clinical interventions based on the patient’s anatomical Delta (Δ) score. As part of the patient data collection process, every patients’ heels and sacrum were scanned once daily during the day shift and each patient’s skin tone was identified using the Fitzpatrick scale. During the evaluation the scanning was performed by the identified group with many of the bedside nurses observing the process and performing an appropriate clinical intervention at the specific anatomical site identified at increased risk of a PI.
Results
Analysis of the data revealed that when it comes to identifying risk, the Provizio SEM Scanner significantly increased the team’s ability to identify which patients were at increased risk of developing a PI at an anatomically specific area and encouraged clinical interventions to alleviate PI risk. Sandy remarked, “I feel the Provizio SEM Scanner is a valuable adjunct to current care practices. It can assist clinicians in their clinical intervention decision making to prevent pressure injuries, reassuring and reinforcing that their decisions are having the intended impact for patients of all skin tones.”
Discussion
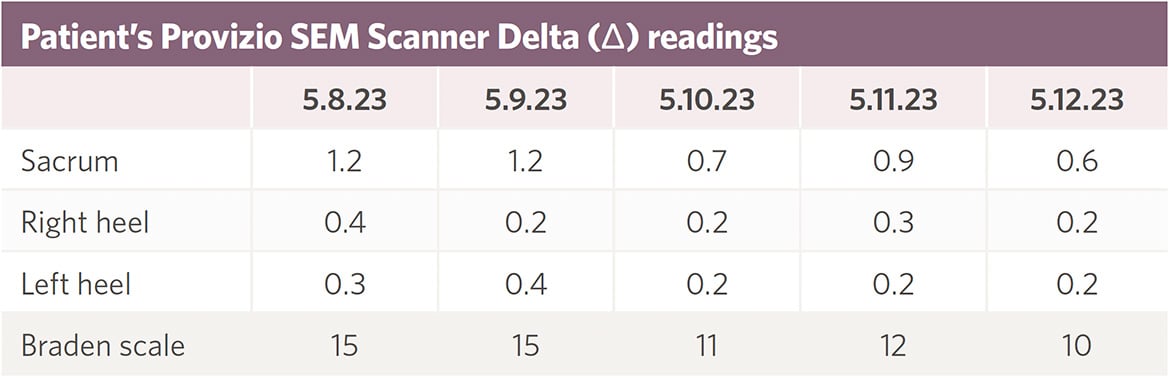 A 74-year old male patient in the SICU with a skin tone Fitzpatrick rating of VI had an initial sacral Delta (Δ) reading indicating he was at increased risk of developing a PI. During his skin assessment, he was noted to have some warmth and hyperpigmentation of the tissue near his sacral region, however his skin was intact. Redness was not seen due to his dark skin tone. His primary nurse was informed that Provizio SEM Scanner identified him at increased risk and clinical intervention to prevent a pressure injury was implemented. The clinical interventions included: repositioning every 2 hours, paying particular attention to ensuring that the sacrum was off-loaded, adhesive foam dressings were placed to his sacrum and both heels, his heels were floated with pillows. As a result both sacrum and bilateral heels remained intact through the entire evaluation period and his sacral Delta (Δ) reading trended down into a “normal” range (Δ < 0.6) due to the timely and targeted clinical measures taken.
A 74-year old male patient in the SICU with a skin tone Fitzpatrick rating of VI had an initial sacral Delta (Δ) reading indicating he was at increased risk of developing a PI. During his skin assessment, he was noted to have some warmth and hyperpigmentation of the tissue near his sacral region, however his skin was intact. Redness was not seen due to his dark skin tone. His primary nurse was informed that Provizio SEM Scanner identified him at increased risk and clinical intervention to prevent a pressure injury was implemented. The clinical interventions included: repositioning every 2 hours, paying particular attention to ensuring that the sacrum was off-loaded, adhesive foam dressings were placed to his sacrum and both heels, his heels were floated with pillows. As a result both sacrum and bilateral heels remained intact through the entire evaluation period and his sacral Delta (Δ) reading trended down into a “normal” range (Δ < 0.6) due to the timely and targeted clinical measures taken.
“As a nursing professional, I am committed to identifying and preventing HAPIs. Using Provizio SEM Scanner as a bedside device with our Nursing staff had a very ‘aha moment’. I felt it recognized the efficacy of the nursing quality of care, confirming that yes, you are giving exceptional care without exception” stated Lauren. The overall reduction of PIs noted post evaluation by the Wound Care team was attributed to the fact that the scanner “had the ability to identify a high delta and changes in the sub-epidermal moisture, even though there was no visible changes present in the targeted areas of heels and sacrum. This allowed our staff to implement PI prevention earlier and the targeted interventions provided offloading of the tissue. This prevented the PI from developing in the patients scanned daily,” concluded Sandy.
The future with continuous improvement
Boston Medical Center has a mission of continuous improvement focused on patient outcomes. The hospital’s goal is to be a leader in the utilization of cutting edge technologies to improve results. BMC has a commitment to provide the best tools for caregivers that aid in enhancing patient and caregiver results. Utilization of the Provizio SEM Scanner is consistent with the BMC mission of exceptional care without exception and its commitment to health equity. The success that BMC had with decreasing PIs in the ICUs has led the Wound Care team to explore the expansion of the utilization of the Provizio SEM Scanner throughout the other patient care units.
If you're interested in reading more, download the full case study here.
The Science of Sub-Epidermal Moisture (SEM) clinical evidence summary
Elevated levels of SEM is a biomarker of early tissue damage that can lead to pressure injury development. SEM can be identified by assessing the biocapacitance of tissue. This noninvasive technology enables early and objective assessment of increased pressure injury (PI) risk, empowering you to take decisive action to minimize PI incidence and to help reduce overall cost and time to care.
Download our Science of SEM clinical evidence summary and learn about:
- The challenges of preventing pressure injuries
- Effects of prolonged pressure on tissue
- The Provizio SEM Scanner hand-held wireless, noninvasive device
- Foundational clinical studies
Download Science of SEM clinical evidence summary
Talk to an Arjo Expert
Learn more about the Provizio SEM Scanner by speaking with an Arjo Expert, who will respond to your request in a timely manner.
References:
- Berlowitz D, VanDeusen Lukas C, Parker V, et al. (Content last reviewed October 2014.) Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. Agency for Healthcare Research and Quality, Rockville, MD. Retrieved from http://www.ahrq.gov/professionals/systems/hospital/pressureulcertoolkit/ index.html.
- Bauer K, Rock K, Nazzal M, Jones O, Qu W, “Pressure Ulcers in the United States’ Inpatient Population From 2008 to 2012: Results of a Retrospective Nationwide Study,” Ostomy Wound Management, November 2016.
- Padula WV, Delarmente BA. The national cost of hospital-acquired pressure injuries in the United States. Int Wound J. 2019 Jun;16(3):634-640. doi: 10.1111/iwj.13071. Epub 2019 Jan 28. PMID: 30693644; PMCID: PMC7948545.
- Redelings, Matthew D et al. “Pressure ulcers: more lethal than we thought?.” Advances in skin & wound care vol. 18.7 (2005): 367-72. doi: 10.1097/00129334-200509000-00010.
- Baumgarten, Mona et al. “Black/White differences in pressure ulcer incidence in nursing home residents.” Journal of the American Geriatrics Society vol. 52.8 (2004): 1293-8. doi: 10.1111.j.1532-5415-2004.52358.x.
- Gunowa, N et al. “Pressure Injuries in People with Dark Skin tones: A Literature Review.” Journal of Clinical Nursing, vol. 27, 2018, pp. 3266-75.
- Gefen A (2018) The future of pressure ulcer prevention is here: Detecting and targeting inflammation early. EWMA Journal 2018, 19(2):7-13.
- Gefen, A (2008). How much time does it take to get a pressure ulcer? Integrated evidence from human, animal and invitro studies. Ostomy Wound Manage. 2008b; 54(10): 26-8,30-5.
- Moore Z., Patton D, Rhodes SL, O’Connor T. Subepidermal moisture and bioimpedance: a literature of novel method for early detection of pressure-induced tissue damage (pressure ulcers). Int Wound J 2017; 14:331-337.
- Dealey C, Posnett J, Walker A. (2012) The cost of pressure ulcers in the UK. Journal of Wound Care, 21 (6):261-266.
- Okonkwo H, Bryant R, Milne J et al. A blinded clinical study using subepidermal moisture biocapacitance measurement device for early detection of pressure injuries. Wound Repair & Reg 2020;1-11.
- Bates-Jensen BM, McCreath HE, Pongquan V. Sub-epidermal moisture is associated with early pressure ulcer damage in nursing home residents with dark skin tones: pilot findings. J Wound Ostomy Continence Nurs.