The importance of time in pressure injury development and how Arjo clinical expertise helps improve outcomes
Pressure injuries (PIs) are one of the largest unsolved healthcare challenges today and International pressure injury prevalence rates are estimated to be between 3-32% in Long Term Care facilities.1 Under certain conditions PIs can begin to develop in a matter of minutes to hours2,7. That is why once an individual’s PI risk is assessed and identified, prescribing the right intervention needs to be fast, simple and straightforward.

The relationship between pressure and time are critical factors in pressure injury development. Research conducted over many years has demonstrated that the magnitude of the mechanical load which may lead to tissue damage depends on the duration of time during which the loads are applied to the skin and tissues2.
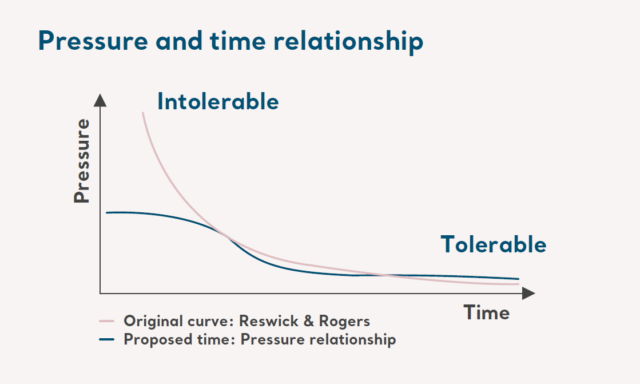
Figure 1
Generally the established principle is that tissue can withstand higher pressures for a short period of time and lower pressures for a longer period7,8,9 (see figure 1). There is no universally ‘safe’ pressure threshold, and it is difficult to determine an absolute time period beyond which a patient will go on to develop a pressure injury8. The speed and severity of the onset of a pressure injury will depend on many internal and external factors including individual anatomy, tissue tolerances and confounding factors2.
Long term care residents and clinical needs vary considerably, and Arjo strives to equip care facilities with skills, tools and solutions to optimize clinical and financial outcomes.
Arjo’s commitment to optimize clinical and financial outcomes
To answer clinical needs in a speedy manner, Arjo, a global leader in the prevention and management of pressure injuries, offers a comprehensive range of rental solutions including medical beds; patient handling solutions; clinical seating; and therapeutic support surfaces, including alternating pressure, foam, low air loss, microclimate management and hybrid systems. With a nationwide network of Rental offices and Service centers it allows to meet the needs of Long Term Care facilities in a timely fashion.
With a full range of wound care solutions for prevention and management of pressure injuries, Arjo supports customers with added clinical expertise, and a high standard of service and education.
Are you looking for a rental solutions partner to support you in effective pressure injury prevention?
When you partner with Arjo for rentals, you collaborate with a Clinical Excellence Team of physical therapists and wound care clinicians. Arjo’s team can support you in providing recommendations based on clinical risk assessments; clinical protocol development and 24/7 education and training resources.
References:
- Anthony, D. M., Alosoumi, D., and Safari, R. (2019). ‘Prevalence of pressure ulcers in long term care: A global review’, Journal of Wound Care, 28(11), pp. 1-7. DOI: 10.12968/jowc.2019.28.11.702.
- Gefen A (2018) The future of pressure ulcer prevention is here: Detecting and targeting inflammation early. EWMA Journal 2018, 19(2):7-13.
- Li Z, Lin F, Thalib L, Chaboyer W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: A systematic review and meta-analysis. Int J Nurs Stud. 2020 May.
- Moore Z, Avsar P, Conaty L, Moore D.H, Patton D, & O’Connor T (2019) The prevalence of pressure ulcers in Europe, what does the European data tell us? Journal of Wound Care.
- Berlowitz D, Lukas CV, Parker V, Niederhauser A, Silver J, Logan Cet al. Preventing pressure ulcers in hospitals: a toolkit for improving quality of care [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; 2014 [cited 2018 Oct 2].
- Anthony, D. M., Alosoumi, D., and Safari, R. (2019). ‘Prevalence of pressure ulcers in long term care: A global review’, Journal of Wound Care, 28(11), pp. 1-7. DOI: 10.12968/jowc.2019.28.11.702.
- Gefen, A (2008). How much time does it take to get a pressure ulcer? Integrated evidence from human, animal and invitro studies. Ostomy Wound Manage. 2008b; 54(10): 26-8,30-5.
- European Pressure Injury Advisory panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Advisory Alliance. The Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed). EPUAP/NPIAP/PPPIA, 2019.
- Linder-Ganz E, Engelberg S, Scheinowitz M, et al. Pressure time cell death threshold for albino rat skeletal muscles as related to pressure sore biomechanics. J Biomech. 2006; 39(14).